“Thanks to recent advances in treatment options including poly ADP ribose polymerase (PARP) inhibitors, the number of women living with their disease as women with epithelial ovarian cancer is growing, with over 40% of patients alive at 5 years.” Logue, Pugh, and Jayson, 2020.
Personal story
This is a “never did I ever” story. Never did I ever anticipate contracting high serous epithelial ovarian cancer–especially not in the first few months of a new, exciting love affair–my first intimacy since 2017. This prolonged period of touch starvation, along with the isolation of the pandemic, and the personal isolation I’ve endured for decades as a person with environmental illness, had all served to disconnect me from my body. It was only with the awakening of love and the resulting restored awareness of my body that I began to notice that there was a “something” that probably needed some attention. I thought it was a inguinal hernia, but ultrasound proved it to be a very swollen lymph node. Very.
On March 15th, 2024, a pathologist confirmed epithelial cells in that lymph node, which meant cancer, one which had metastasized to the lymph system and possibly elsewhere. Color me shocked!
I was lucky to push through the Kaiser bureaucracy for a CT scan three days later. Results showed that matters were even worse than I expected. What followed were weeks of more bureaucratic frustration as the Kaiser Permanente referral department and various outside providers kept dropping my case into various Catch-22 situations which resulted in delay after delay after delay. All I wanted was to see an oncologist and start treatment ASAP. (Can you spell “argh?”)
Unless you’ve been in a similar situation, it’s hard to imagine the combination of frustration, anguish, anger, depression, exhaustion, and sheer existential sorrow that those weeks held for me. I was under a death sentence of sorts, just when I wanted so much to live and love again. I was flush with the joys of a tender new love but preparing myself for an unquiet grave at the same time. No, I am not being dramatic. Such situations naturally engender and even require strong, conflicting emotions.
When I was finally accepted as a patient at a local (and very excellent) cancer treatment center, one of the first things the oncologist said to me was that she could offer me hospice. Again, my reaction was one of shock. And then, after I’d been given a moment to reel from the blow, she offered treatment options. I am not sure of the kindness of that particular method of prognosis delivery, but it did make an impression. And, it’s interesting that this did not shake my trust in her but actually strengthened it.
I must be peculiar.
As for hospice, hell no I won’t go! Give me what it takes to survive.
And of course I was worried as to whether my new relationship would survive as well. Many of us have been sadly let down in times of duress by people who have said they love us, and I am no exception. Of course I had fears. But so far those fears have been groundless. In fact, I can say that I am supported in this weird, rough time with more emotional commitment than I could have imagined, though there are logistical constraints.
Fast forward to now, a few months down the road: three rounds of chemotherapy which have been rough but quite, quite efficacious, allowing the cancerous areas to shrink enough to enable me to have robotic assisted laparoscopic hysterectomy, bilateral salpingo-oopherectomy, omentectomy, and tumor debulking! This happened at the end of June and I am doing quite well, remarkably well, considering. Coming up: three more rounds of chemo, and then we’ll see what’s what with another CT scan and labs.
I know that living as “a survivor” will be a major context of my future. That’s okay. I want five years and more. I want a robust remission and by golly, I’ll work my patoosis off for it.
However I sure hate being bald and I have so many practical questions. More on those later.
Now to the sexological portion of this blog post…
Common problems in sexual behavior and function
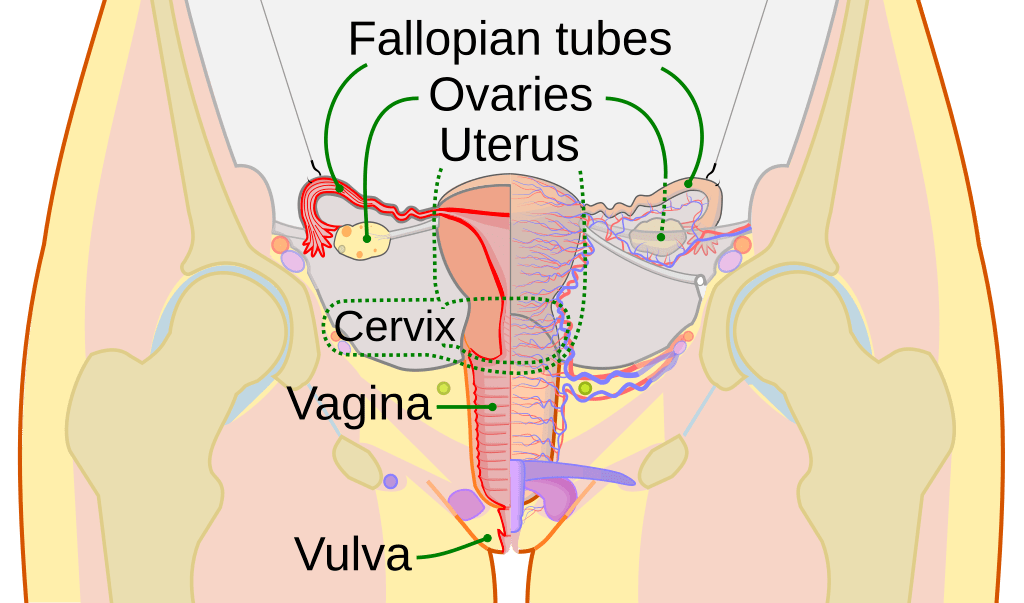
Vaginal dryness, body image issues, early menopause (for those who are diagnosed and treated prior to natural menopause), low levels of desire, pain with intercourse: these are just a few of the difficulties faced by people who have undergone treatment for ovarian cancer. Other issues include changes to and stresses upon intimate relationships, worries about desirability, and many other complexities that tend to undermine sexual confidence and pleasure.
Here’s a screenshot from a study that describes some of the sexual challenges:

In future blogs I’ll be addressing specific concerns as described in many of the studies below. I’ll also share some of my own personal challenges and worries, as I think I may not be alone in experiencing them. Perhaps it will help other people if I can articulate some of them.
Ovarian Cancer & Sexuality Studies
Bober, S.L., Recklitis, C.J., Michaud, A.L. and Wright, A.A. (2018), Improvement in sexual function after ovarian cancer: Effects of sexual therapy and rehabilitation after treatment for ovarian cancer. Cancer, 124: 176-182. https://doi.org/10.1002/cncr.30976
Fischer, Olivia J., Monique Marguerie, and Lori A. Brotto. “Sexual function, quality of life, and experiences of women with ovarian cancer: a mixed-methods study.” Sexual medicine 7.4 (2019): 530-539.
Kim, Se Ik, et al. “Quality of life and sexuality comparison between sexually active ovarian cancer survivors and healthy women.” Journal of gynecologic oncology 26.2 (2015): 148.
Logue, Chloe Alice, Julia Pugh, and Gordon Jayson. “Psychosexual morbidity in women with ovarian cancer.” International Journal of Gynecologic Cancer 30.12 (2020).
Mayer, Sebastian, et al. “Sexual activity and quality of life in patients after treatment for breast and ovarian cancer.” Archives of gynecology and obstetrics 299 (2019): 191-201.
Stead, Maxine L., et al. “Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues.” British journal of cancer 88.5 (2003): 666-671.
Whicker, Margaret, et al. “Management of sexuality, intimacy, and menopause symptoms in patients with ovarian cancer.” American journal of obstetrics and gynecology 217.4 (2017): 395-403.
Breast Cancer & Sexuality Studies
A lot of work has been done on sexual concerns of breast cancer patients and there are some similarities with ovarian cancer patients. Below are just three of the many studies that may be found.
Emilee, Gilbert, Jane M. Ussher, and Janette Perz. “Sexuality after breast cancer: a review.” Maturitas 66.4 (2010): 397-407.
Fleming, Megan P., and Elaine Kleinbart. “Breast cancer and sexuality.” Journal of sex Education and Therapy 26.3 (2001): 215-224.
Ussher, Jane M., Janette Perz, and Emilee Gilbert. “Changes to sexual well-being and intimacy after breast cancer.” Cancer nursing 35.6 (2012): 456-465.
Needed: More info on the clinical importance of sexual pleasure
A few months ago I came across a study that claimed that female and female-bodied breast cancer patients who were sexually active had a better prognosis. I found it once and need to find it again. At the time, this finding indicated (to me) the importance of PLEASURE and intimate connection in healing and maintaining health.

Really sorry to read this news. I admire your determination to go full on with chemo and surgery rather than just give up. Hoping the best for you throughout the process. John Kamp
LikeLike
Thank you!
LikeLike